Obesity & Cardiovascular Disease
How can obesity raise the chance of cardiovascular and other diseases? Obesity and Cardiovascular Disease are connected. Being overweight, particularly around the waist, can cause fat to accumulate in your arteries, which are the blood vessels that supply blood to your organs. We call this atherosclerosis.
Additionally, it may raise your risk of type 2 diabetes, high blood pressure, and high cholesterol. Heart disease risk factors also include these.
A heart attack may result from clogged and damaged arteries that provide blood to the heart. A stroke or vascular dementia may result if this occurs in the arteries supplying blood to the brain.
Follow the best way to take Vitamin and Mineral Supplements
Body Composition & Fat
The body contains a variety of fat kinds. A lot of individuals are concerned about the visceral fat that lies beneath the skin. We refer to this as subcutaneous fat.
However, visceral fat, a different kind of fat, poses a greater risk to health. This surrounds our internal organs, including the liver and heart, and influences how well our blood arteries and heart work. To maintain some space between our organs, it is normal to retain some visceral fat.
On the other hand, excess visceral fat can:
- Increase cholesterol levels in your blood.
- Raise your blood pressure and you run the greater chance of getting type 2 diabetes.
- Heart and circulation disorders are strongly associated with each of these risk factors.
Heart Disease Associated with Obesity
Obesity and heart problems are associated with several types of difficulties:
Coronary artery disease: The accumulation of cholesterol plaque in the heart’s arteries causes coronary artery disease (CAD), which is exacerbated by obesity. Obesity is a risk factor for CAD even though it is associated with numerous other risk factors, including metabolic syndrome, high blood pressure, high cholesterol, and diabetes. People with “central” or “visceral” obesity—obesity that is located in the abdomen—have an increased risk of developing CAD.
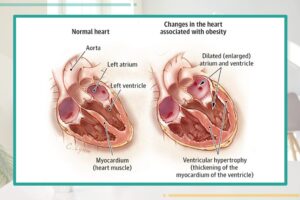
Obesity and heart failure: Even in those without CAD, obesity raises the chance of developing heart failure. Although the precise mechanism by which obesity may lead to heart failure in the absence of CAD is unknown, there are two primary theories. First, those who are obese typically have larger blood volumes, which over time can cause the heart to beat more forcefully and eventually result in heart failure. Ventricular hypertrophy is the term for the situation when the heart becomes larger due to increased workload. Second, obesity and sleep apnea are associated with high blood pressure and lung issues, both of which can eventually result in heart failure.
Sudden cardiac death: Research has indicated that obesity increases the risk of sudden cardiac death even in those who do not have coronary artery disease (CAD), heart failure, or other heart diseases.
Obesity has been linked to an increased risk of atrial fibrillation, a heart rhythm abnormality, according to numerous research. Atrial fibrillation is frequently observed in heart failure patients. As a result, there are strong connections between the pathways including atrial fibrillation, cardiac failure, and obesity. A study in this issue of JAMA describes how losing weight can lessen atrial fibrillation-related issues.
Effect of Obesity on Heart
Obesity, particularly abdominal obesity, has profound effects on cardiovascular health. The accumulation of excess fat, especially around the abdomen, significantly increases the risk of heart disease and related complications. This condition is not just a cosmetic concern; it is a critical health issue that can lead to severe cardiovascular events, including heart attacks and strokes.
Understanding Obesity Types
Obesity is generally classified into two types: subcutaneous fat (fat stored under the skin) and visceral fat (fat stored around internal organs). While both types can contribute to health risks, visceral fat is particularly harmful due to its close association with metabolic dysfunction and inflammation. Abdominal obesity is typically assessed using waist circumference and waist-to-hip ratio, which are effective indicators of visceral fat accumulation.
Mechanisms Linking Obesity to Heart Disease
Inflammation: Excess visceral fat releases pro-inflammatory cytokines, which can lead to chronic inflammation. This inflammatory state contributes to endothelial dysfunction, a condition where the blood vessels become less able to regulate blood flow, increasing the risk of atherosclerosis and heart disease.
Lipid Profile Alterations: Obesity often results in dyslipidemia, characterized by elevated levels of low-density lipoprotein (LDL) cholesterol and triglycerides, along with reduced high-density lipoprotein (HDL) cholesterol. This imbalance can accelerate the development of atherosclerosis, leading to narrowed arteries and reduced blood flow to the heart.
Insulin Resistance: Abdominal obesity is closely linked to insulin resistance, which can lead to type 2 diabetes. Insulin resistance increases the risk of cardiovascular disease by promoting hypertension, dyslipidemia, and inflammation.
Hypertension: Obesity is a significant risk factor for high blood pressure, which places additional strain on the heart and blood vessels. Over time, this can lead to left ventricular hypertrophy (thickening of the heart’s walls), increasing the risk of heart failure.
Cardiac Remodeling: The heart may undergo structural changes due to chronic obesity and associated conditions, such as hypertension and diabetes. These changes can impair cardiac function and increase the likelihood of arrhythmias.
The Risk of Heart Attacks
Individuals with obesity face a markedly higher risk of experiencing heart attacks. The presence of excess abdominal fat not only increases the likelihood of a first heart attack but also raises the risk of subsequent heart events. Studies have shown that those with significant abdominal fat are more prone to recurrent cardiac issues due to the persistent effects of inflammation, metabolic dysfunction, and poor adherence to treatment.
Strategies for Mitigating Risks
Addressing obesity and its impact on heart health is crucial for prevention and management. Effective strategies include:
Nutritional Interventions: Adopting a heart-healthy diet that emphasizes whole foods, such as fruits, vegetables, whole grains, lean proteins, and healthy fats, can help reduce visceral fat and improve overall cardiovascular health.
Regular Physical Activity: Engaging in regular exercise, including aerobic and strength training, is vital for weight management and improving heart health. Physical activity helps reduce abdominal fat, lowers blood pressure, and enhances lipid profiles.
Behavioral Support: Programs that focus on lifestyle changes can provide individuals with the necessary tools and motivation to maintain healthy habits, improving adherence to dietary and exercise recommendations.
Monitoring and Screening: Regular assessments of weight, waist circumference, and metabolic health markers can help identify individuals at risk for heart disease and facilitate timely interventions.
Abdominal Obesity and Heart Disease
Abdominal obesity, characterized by excess fat accumulation around the abdomen, has long been recognized as a risk factor for various health issues, particularly cardiovascular diseases. While extensive research has established the connection between excess stomach fat and an increased risk of having a first heart attack, emerging studies suggest that this form of obesity poses an even greater threat: it may significantly elevate the risk of repeat heart attacks.
Understanding Abdominal Obesity
Abdominal obesity is typically measured by waist circumference and waist-to-hip ratio, indicators that reflect the distribution of body fat. Unlike subcutaneous fat found under the skin, visceral fat, which surrounds internal organs, plays a critical role in metabolic processes and inflates inflammation and insulin resistance levels. This is particularly concerning because visceral fat is more closely linked to various health risks, including heart disease.
Read about the Wide Bulbous Nose Surgery
The Risk of a First Heart Attack
The mechanisms linking abdominal obesity to heart disease are multifaceted. Excess visceral fat can lead to increased levels of inflammatory markers, changes in lipid profiles, and alterations in blood glucose metabolism. These factors contribute to atherosclerosis, the process by which plaque builds up in the arteries, narrowing them and making it harder for blood to flow. This can ultimately result in a heart attack.
The Increased Risk of Recurrent Heart Attacks
Recent research has illuminated a concerning trend: individuals with significant abdominal fat not only face a heightened risk of their first heart attack but are also at a greater risk of experiencing additional cardiac events. Studies indicate that those with abdominal obesity are more likely to suffer from recurring heart problems, including subsequent heart attacks. Compared to their counterparts with a more favorable fat distribution.
The reasons behind this increased risk are still under investigation, but they may involve:
Persistent Inflammation: Individuals with abdominal obesity often have chronic inflammation due to the excess visceral fat, leading to ongoing damage to blood vessels and the heart.
Metabolic Dysfunction: Abdominal obesity is associated with metabolic syndrome, a cluster of conditions—including high blood pressure, elevated blood sugar levels, and abnormal cholesterol levels—that collectively escalate cardiovascular risk.
Poor adherence to Treatment: After a first heart attack, maintaining a heart-healthy lifestyle can be challenging. Those with abdominal obesity may struggle more with dietary modifications and physical activity, hindering recovery and increasing recurrence chances.
Medication Efficacy: There is evidence to suggest that visceral fat can alter how the body responds to medications, potentially reducing the effectiveness of treatments prescribed post-heart attack.
Obesity and Heart Disease
Given the alarming link between abdominal obesity and repeat heart attacks. It is crucial for healthcare professionals to emphasize weight management strategies focusing on reducing abdominal fat. Effective measures include:
Dietary Changes: Encouraging a heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can help reduce visceral fat.
Regular Exercise: Engaging in regular physical activity, including cardiovascular and strength training exercises. It`s vital for reducing abdominal fat and overall heart health.
Behavioral Interventions: Programs that support lifestyle changes can provide the necessary tools and motivation for individuals to maintain healthy habits.
Routine Monitoring: Regular assessments of waist circumference and metabolic health markers can help identify individuals at risk and initiate timely interventions.
Conclusion
As research continues to uncover the intricate relationship between abdominal obesity and heart disease. Particularly the risk of subsequent heart attacks. It becomes evident that addressing this specific form of obesity is essential for cardiovascular health. With a proactive approach to weight management and lifestyle changes. Individuals can mitigate their risk and promote healthier outcomes for their hearts.